What Is the Science Behind Gene Editing in Medicine
 Health & medical treatment
Health & medical treatment Gene editing has become a cornerstone of modern medicine, offering innovative solutions to some of the most challenging diseases. While altering DNA may seem like science fiction to some, it is now a robust and rapidly advancing tool in healthcare. The key technology driving this revolution is CRISPR-Cas9, which allows scientists to make precise changes to an organism's genetic code. However, gene editing is not just a genetic breakthrough; it promises to change how we treat genetic disorders, cancers, and viruses. In this article, we explore the science behind gene editing, its current medical applications, and the hurdles that remain as researchers refine these techniques.
Gene editing has become a cornerstone of modern medicine, offering innovative solutions to some of the most challenging diseases. While altering DNA may seem like science fiction to some, it is now a robust and rapidly advancing tool in healthcare. The key technology driving this revolution is CRISPR-Cas9, which allows scientists to make precise changes to an organism's genetic code. However, gene editing is not just a genetic breakthrough; it promises to change how we treat genetic disorders, cancers, and viruses. In this article, we explore the science behind gene editing, its current medical applications, and the hurdles that remain as researchers refine these techniques.
What Is Gene Editing?
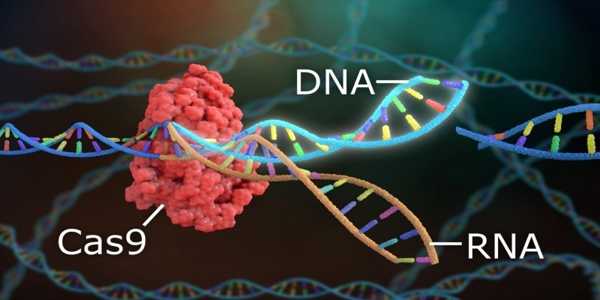
Gene editing refers to making specific changes to the DNA within a cell's genome. These alterations can involve adding, removing, or modifying genetic material to correct mutations that cause diseases. The most famous gene-editing tool today is CRISPR-Cas9, derived from a natural defence mechanism found in bacteria. When viruses attack bacteria, they store pieces of viral DNA in their genome to help recognize and fight off future infections. Scientists adapted this process to cut DNA at precise locations, allowing them to change the genetic material of various organisms, including humans.
The precision and versatility of CRISPR have propelled it to the forefront of gene editing, particularly in medicine. However, other methods, such as prime editing and base editing, have also emerged as potential alternatives or improvements to CRISPR, especially for making more accurate or less disruptive edits.
Gene Editing In Medicine: Current Applications
The application of gene editing in medicine is vast, with potential treatments for various conditions. Here are some of the most notable areas where gene editing is making an impact:
Genetic Disorders
Gene editing has shown immense promise in treating genetic disorders by directly altering the genes that cause these diseases. Conditions like sickle cell disease, cystic fibrosis, and Duchenne muscular dystrophy, all caused by mutations in a single gene, are prime candidates for gene-editing therapies.

One of the most notable successes in this area is using CRISPR to treat sickle cell disease. In 2023, the FDA approved a CRISPR-based sickle cell therapy developed by Vertex Pharmaceuticals and CRISPR Therapeutics. This treatment involves extracting blood stem cells from patients, editing the cells to correct the genetic mutation, and reinfusing the edited cells back into the patient. The results have been transformative, with many patients experiencing significant reductions in the painful episodes and complications associated with the disease.
Cancer Treatment
Cancer, with its roots in genetic mutations, is another area where gene editing holds great promise. The ability to alter the genetic makeup of cancer cells could lead to therapies that target and destroy tumours more effectively. Recent research focuses on gene editing to modify immune cells, such as T-cells, to recognize and attack cancer cells. Clinical trials using CRISPR-edited immune cells have already successfully treated certain types of cancer, including blood cancers like leukaemia.

Additionally, researchers are investigating ways to directly edit the genes of cancer cells to either reverse mutations or make them more susceptible to other treatments, such as chemotherapy and immunotherapy.
Viral Diseases
Gene editing is also showing promise in the fight against viral diseases, including HIV and potentially even more complex viruses like the hepatitis B virus (HBV). Researchers have successfully used CRISPR to target and disrupt the DNA of HIV in human cells, essentially "curing" the infection in a lab setting. While these findings are still in the early stages, they open the door for developing gene therapies that could offer long-term solutions for viral infections.
Hereditary Diseases And Rare Disorders
Gene editing is being explored as a potential treatment for rare and hereditary diseases, as well as common genetic disorders. For example, conditions like haemophilia and certain inherited blindness are caused by specific mutations in a single gene. By correcting or replacing these faulty genes, gene editing could provide a permanent solution for patients who currently have no effective treatments.

Clinical trials are underway in 2024 for diseases such as hereditary angioedema, in which CRISPR is used to reduce inflammatory protein levels that cause severe swelling.
Challenges In Gene Editing For Medicine
Despite its promise, gene editing in medicine is challenging. Several obstacles need to be addressed before these therapies can become widespread.
Delivery Mechanisms
One of the biggest hurdles in gene editing is finding a safe and efficient way to deliver the editing tools to the target cells in the human body. Traditionally, gene editing requires extracting cells from the patient, editing them in the lab, and then reinfusing them into the patient's body. This process is time-consuming and expensive and carries risks associated with manipulating the cells outside the body.
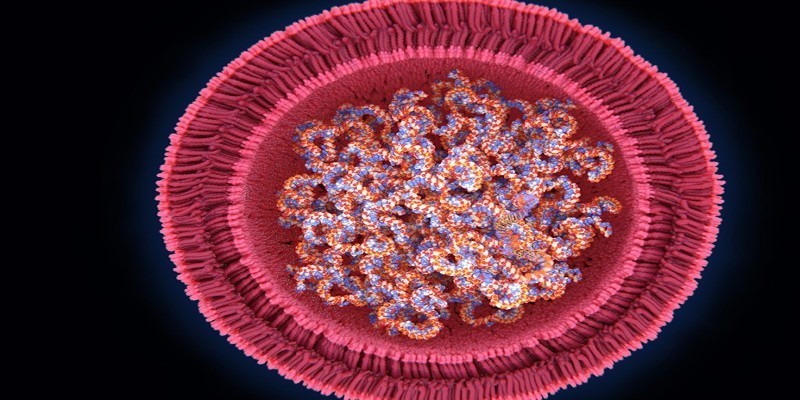
Recently, there has been a concerted effort to develop delivery systems that allow gene editing to occur directly inside the body without needing to remove cells. Lipid nanoparticles and viral vectors are two approaches currently being explored. For example, the treatment for hereditary angioedema mentioned earlier uses lipid nanoparticles to deliver CRISPR components intravenously to the liver, where the disease-causing proteins are made.
Off-Target Effects
Another significant concern with gene editing is the possibility of off-target effects, where the editing tools make unintended changes to the DNA. Even minor errors in the editing process could have serious consequences, such as triggering cancer or other diseases. To minimize these risks, researchers are continually refining the precision of gene editing tools, such as prime editing, which has been shown to make fewer off-target changes than traditional CRISPR.

Additionally, there are concerns about access to gene-editing therapies. Many of the treatments in development are relatively inexpensive, limiting access to those who can afford them. Making gene editing accessible and equitable is a significant challenge that needs to be addressed as the field advances.
The Future Of Gene Editing In Medicine
The future of gene editing in medicine is full of potential. Scientists are actively working to improve gene editing technologies' accuracy, efficiency, and safety. With further advancements in delivery methods and a better understanding of the human genome, gene editing could eventually become a routine treatment for various conditions, from genetic disorders to cancers and viral infections.
